Photos of Megan’s induction into the American Society for Clinical Investigation.
Megan is inducted into the American Society for Clinical Investigation


Photos of Megan’s induction into the American Society for Clinical Investigation.

Some photos of the Dr. Cimpean’s hooding event.


Jalalah Muhammed, Sammy Risma, and Nathan Schedler join the Cooper lab this summer! Welcome!


Megan Cooper, MD, PhD, is a pediatric rheumatologist/immunologist at St. Louis Children’s Hospital. She is the Director of Clinical Immunology at Children’s and an Associate Director of the Medical Scientist Training Program at Washington University School of Medicine. She received her MD and PhD from The Ohio State University before coming to Washington University School of Medicine in St. Louis for her pediatric residency and fellowship in pediatric rheumatology. Currently, her lab focuses on elucidating mechanisms of immune cell control with an interest in both natural killer (NK) cell activation and the molecular mechanisms of pediatric immune-mediated disease.
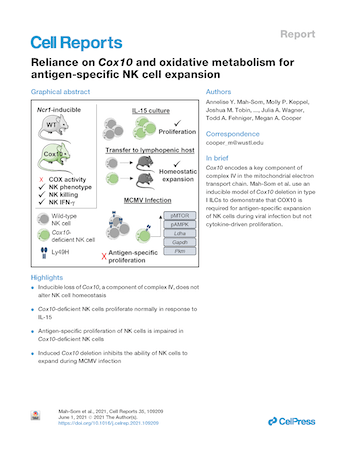
Cox10 encodes a key component of complex IV in the mitochondrial electron transport chain. Mah-Som et al. use an inducible model of Cox10 deletion in type I ILCs to demonstrate that COX10 is required for antigen-specific expansion of NK cells during viral infection but not cytokine-driven proliferation.

Check out the backstory on the brave patients and families that made Jahnavi’s May 2021 published study possible.

Four-year-old Joseph Anthony Vena IV died last year of a rare genetic disease that attacks children’s immune systems. The disease and the genetic mutation that causes it were identified by Megan A. Cooper, MD, PhD, an associate professor of pediatrics at Washington University School of Medicine in St. Louis, working with other researchers. Cooper, who also treats patients at St. Louis Children’s Hospital, specializes in diagnosing and treating rare genetic diseases affecting the immune system. The new discoveries have inspired an ongoing collaboration of scientists nationwide.
1) Jahnavi discusses the new #IEI associated with TLR8 at the Clinical Immunology Society 2021 Meeting!,
2) Erica presents interesting findings on Tregs in STAT3 Gain-of-function at CIS 2021!,
3) Kelsey presents her work on Th17s and STAT3 at the 2021 AAI meeting
and 4) Maria talks about how NK cells are primed by IL-15 at AAI 2021 meeting! Congratulations to all!

Primary immunodeficiency diseases (PIDs) are a rapidly growing, heterogeneous group of genetically determined diseases characterized by defects in the immune system. While individually rare, collectively PIDs affect between 1/1,000 and 1/5,000 people worldwide. The clinical manifestations of PIDs vary from susceptibility to infections to autoimmunity and bone marrow failure. Our understanding of the human immune response has advanced by investigation and discovery of genetic mechanisms of PIDs. Studying patients with isolated genetic variants in proteins that participate in complex signaling pathways has led to an enhanced understanding of host response to infection, and mechanisms of autoimmunity and autoinflammation. Identifying genetic mechanisms of PIDs not only furthers immunological knowledge but also benefits patients by dictating targeted therapies or hematopoietic stem cell transplantation. Here, we highlight several of these areas in the field of primary immunodeficiency, with a focus on the most recent advances.

From the moment Weston was born, he was adored by his parents, Emily and Shane. However, when Weston was just 7-months-old, things began to spiral out of control. Within a three week span, Weston went from a healthy, symptom free child to getting a diagnosis that would change his life.
Washington University School of Medicine in St. Louis is one of more than 30 genome sequencing hubs worldwide participating in a study to sequence the DNA of young, healthy adults and children who develop severe COVID-19 despite having no underlying medical problems. The researchers also will study people who never become infected despite repeated exposures to coronavirus. Knowledge gained from understanding COVID-19’s extremes could lead to new therapeutic strategies for the illness.
Annelise graduates and moves to Boston where she will be an Internal Medicine resident! Congratulations Annelise!

On the outside, Parker looks like any other kid. However, common illnesses can quickly turn very serious for him. There are less than 70 cases of his disease documented in the world. Without access to St. Louis Children’s Hospital and the Children’s Discovery Institute, it is unlikely Parker’s family would have been able to get any answers.

Megan and Maria travel to Luxembourg for the NK meeting and present work from the lab!



Molly receives the Shooting Star Award from the Department of Pediatrics for excellence in Research
Tiphanie graduates from fellowship and the lab and moves to Baylor to start her own research program!
Megan presents the laboratory’s work on STAT3 at the American College of Rheumatology Annual Meeting